CASE20250516_002
TAVI in a Destroyed Lung
By Hendrianus , Sang-Wook Kim
Presenter
Hendrianus
Authors
Hendrianus 1, Sang-Wook Kim2
Affiliation
Chung-Ang University Gwangmyeong Hospital, Indonesia1, Chung-Ang University Gwangmyeong Hospital, Korea (Republic of)2,
View Study Report
CASE20250516_002
TAVR - Complex TAVR
TAVI in a Destroyed Lung
Hendrianus 1, Sang-Wook Kim2
Chung-Ang University Gwangmyeong Hospital, Indonesia1, Chung-Ang University Gwangmyeong Hospital, Korea (Republic of)2,
Clinical Information
Relevant Clinical History and Physical Exam
A 65-year-old female with advanced COPD and prior pulmonary tuberculosis presented with worsening exertional dyspnea. Examination showed decreased breath sounds bilaterally and a systolic murmur at the right upper sternal border. Chest X-ray revealed hyperinflated lungs with diffuse fibrotic changes, cavitary lesions, and calcified nodular infiltrates, consistent with post-tuberculous destroyed lung syndrome.


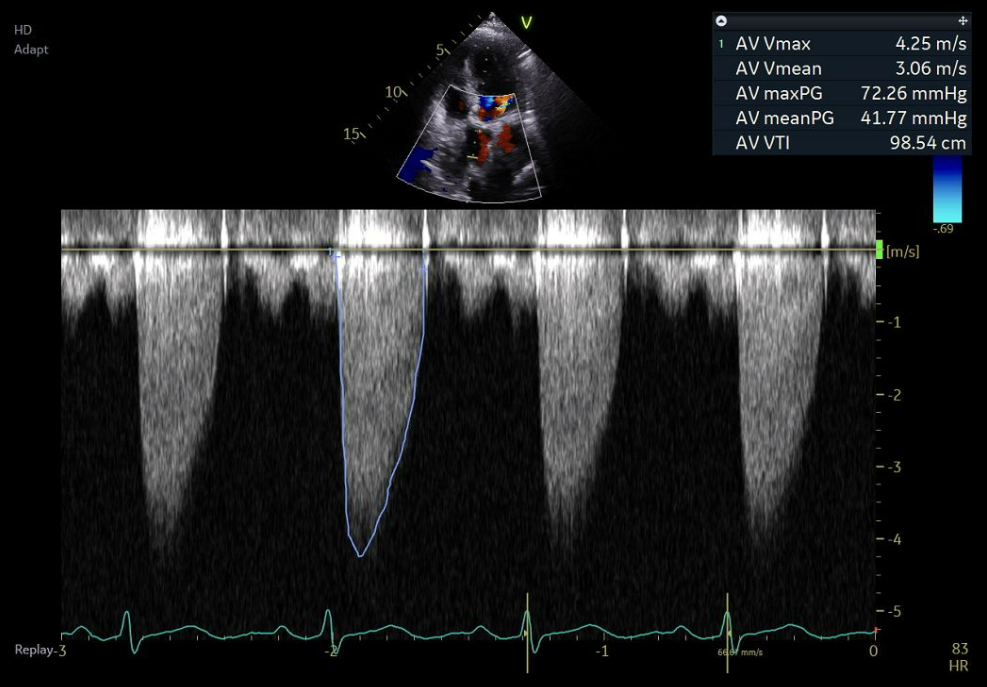
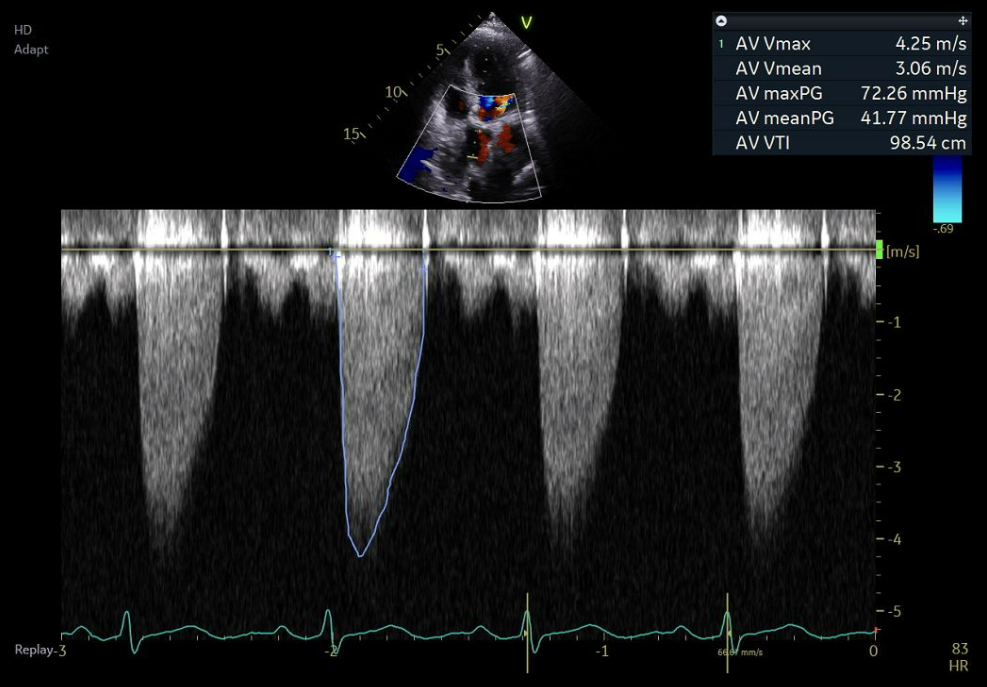
Relevant Test Results Prior to Catheterization
Transthoracic echocardiography revealed an LVEF of 58%, progression of aortic stenosis (AV Vmax 3.7→4.3 m/s; mean gradient 37→42 mmHg; AVA 1.17→0.98 cm²), and worsening tricuspid regurgitation (mild to moderate) with signs of pulmonary hypertension. Preprocedural MSCT showed favorable transfemoral access and anatomy suitable for TAVI, with an annulus diameter of 21.3 mm.
 이향분000310592025-02-1402.wmv
이향분000310592025-02-1402.wmv
 이향분000310592025-02-1409.wmv
이향분000310592025-02-1409.wmv
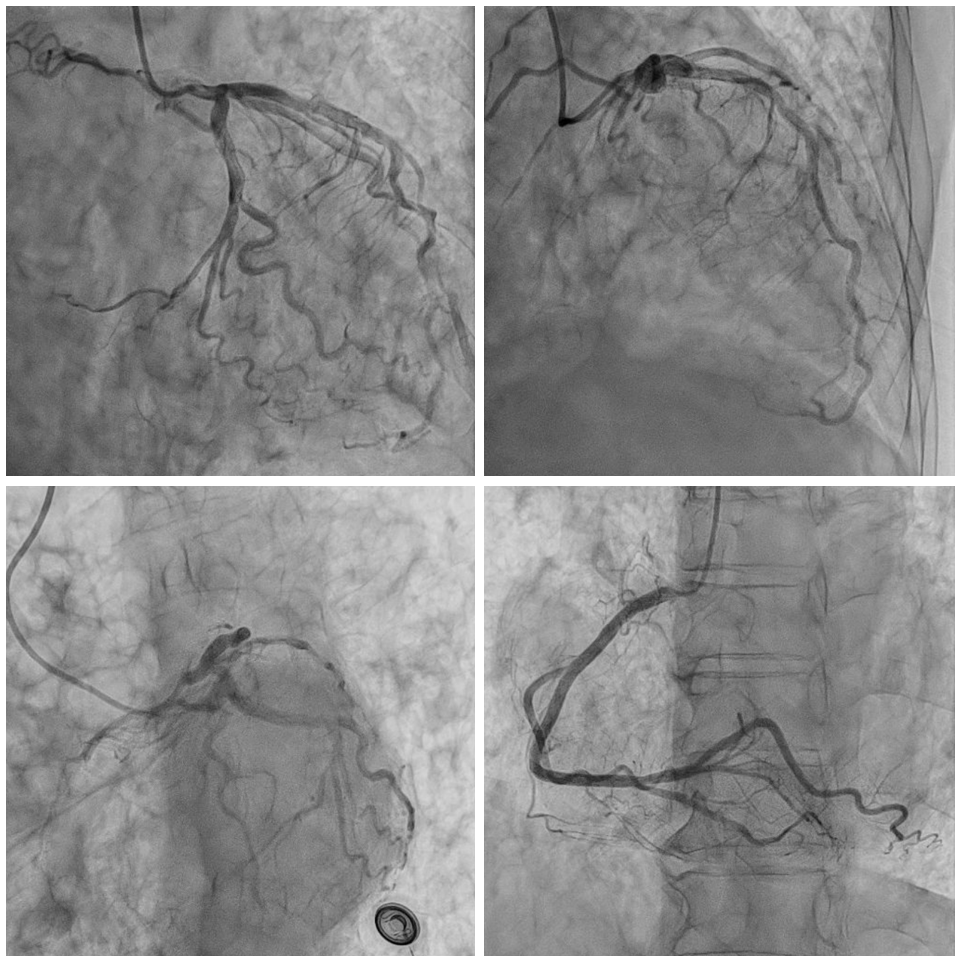
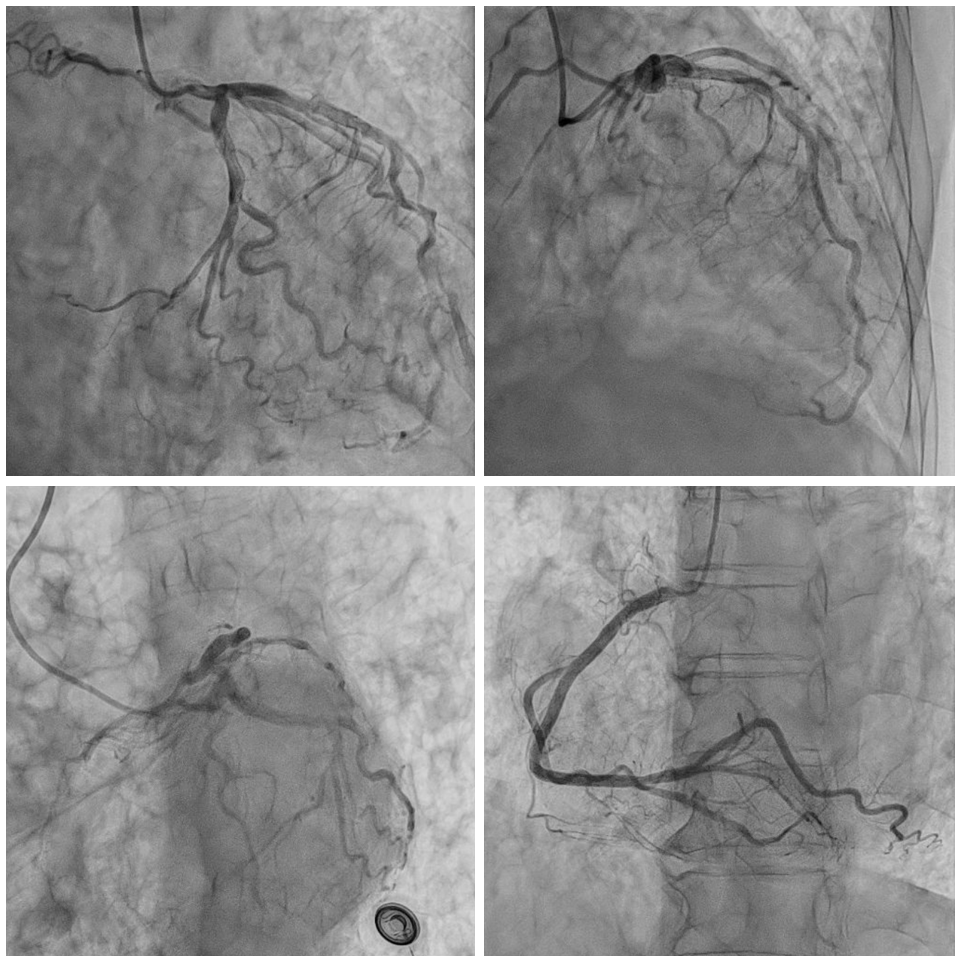
Relevant Catheterization Findings
Coronary angiography performed one week prior to TAVI showed non-obstructive coronary artery disease and revealed a fistula from the proximal LAD to the pulmonary trunk.
Interventional Management
Procedural Step
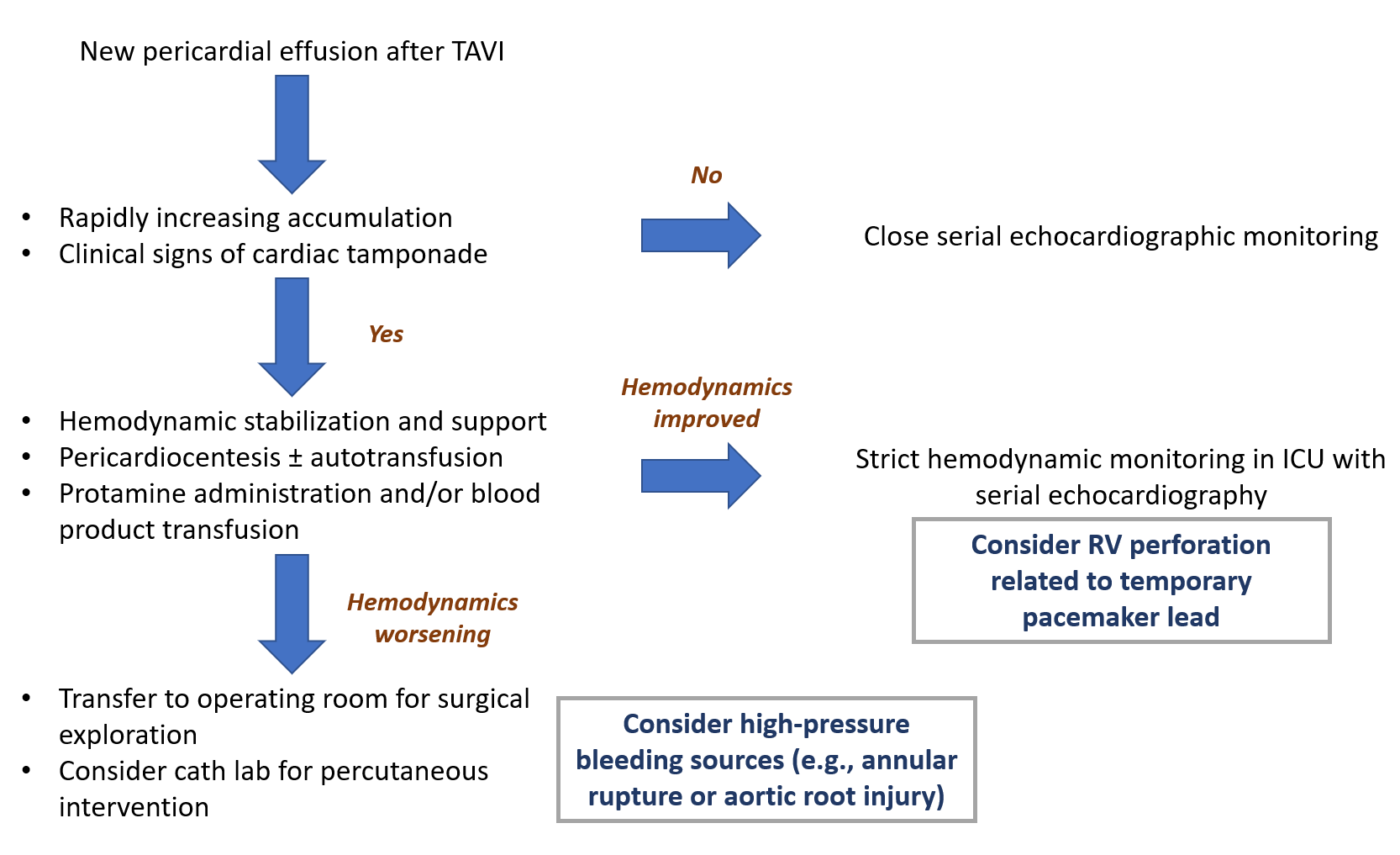
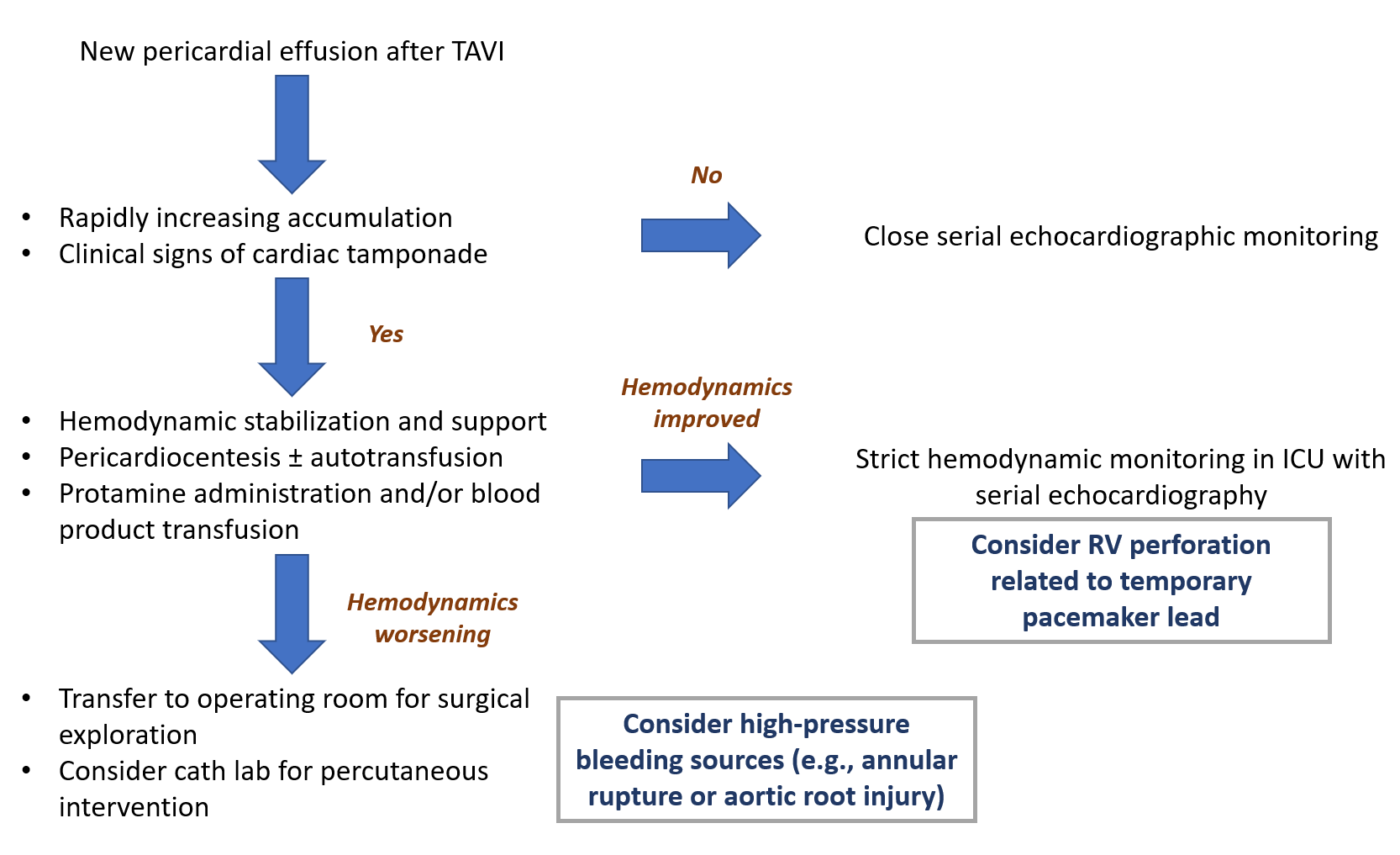
The procedure was performed under local anesthesia. Transfemoral TAVI was carried out via the right common femoral artery using an 18 Fr sheath, and a 26 mm self-expanding CoreValve Evolut Pro was implanted. ICE guidance was obtained via the left femoral vein, and a temporary pacemaker was positioned at the right ventricular apex through the right femoral vein with a stable threshold of <1.5 V. The patient developed frequent coughing during the procedure, which caused technical difficulty during valve deployment and necessitated three recaptures before successful release. ICE confirmed optimal valve position, minimal paravalvular leak, and no significant effusion. Aortography showed no contrast extravasation. One hour post-procedure, echocardiography revealed rapidly increasing pericardial effusion with signs of impending tamponade. Emergent pericardiocentesis drained ~250 mL of hemorrhagic fluid. Annular rupture or aortic root injury was initially suspected, and surgical backup was activated. However, these were later deemed unlikely due to the patient’s relative hemodynamic stability following pericardiocentesis. She remained stable in the ICU under surgical standby. RV perforation from the pacing lead was considered the most likely cause. The drain was removed on day 5. She was discharged on day 10. At 3-month follow-up, echocardiography showed no pericardial effusion, no paravalvular leak, and a well-functioning prosthetic valve with a mean aortic gradient of 9 mmHg.
 1.2.840.113619.2.435.390867136.1739280388.71.1.512.dcm.wmv
1.2.840.113619.2.435.390867136.1739280388.71.1.512.dcm.wmv


Case Summary
This case highlights a rare but life-threatening early cardiac tamponade following TAVI in a patient with severely compromised pulmonary anatomy. The most plausible mechanism is cough-induced RV perforation by the pacing lead, despite optimal lead positioning and low capture threshold. Repeated coughing may have generated surges in intrathoracic pressure, forcing the thin RV wall against the lead tip. The absence of contrast extravasation on final aortography and rapid stabilization with conservative management support this diagnosis. Anatomical challenges, such as a destroyed lung, necessitate heightened procedural vigilance and tailored strategies to mitigate risk.
