CASE20250515_002
Alcohol Septal Ablation for Relieving Dynamic Left Ventricular Outflow Tract Obstruction Following Transcatheter Aortic Valve Replacement
By Yonghoon Shin, Mi-Na Kim, Ha Young Yu, Jung-Joon Cha, Hyung Joon Joo, Jae Hyoung Park, Soon Jun Hong, Cheol Woong Yu
Presenter
Yonghoon Shin
Authors
Yonghoon Shin1, Mi-Na Kim1, Ha Young Yu1, Jung-Joon Cha1, Hyung Joon Joo1, Jae Hyoung Park1, Soon Jun Hong1, Cheol Woong Yu1
Affiliation
Korea University Anam Hospital, Korea (Republic of)1,
View Study Report
CASE20250515_002
Other Interventions - Other Interventions
Alcohol Septal Ablation for Relieving Dynamic Left Ventricular Outflow Tract Obstruction Following Transcatheter Aortic Valve Replacement
Yonghoon Shin1, Mi-Na Kim1, Ha Young Yu1, Jung-Joon Cha1, Hyung Joon Joo1, Jae Hyoung Park1, Soon Jun Hong1, Cheol Woong Yu1
Korea University Anam Hospital, Korea (Republic of)1,
Clinical Information
Relevant Clinical History and Physical Exam
A 98-year-old female presented with syncope while ambulating 10 days prior to admission. Physical examination revealed a grade III/VI systolic ejection murmur best auscultated at the left sternal border. Her past medical history was significant for hypertension, persistent atrial fibrillation, and transcatheter aortic valve replacement (TAVR) for severe aortic stenosis 6 years prior.
Relevant Test Results Prior to Catheterization
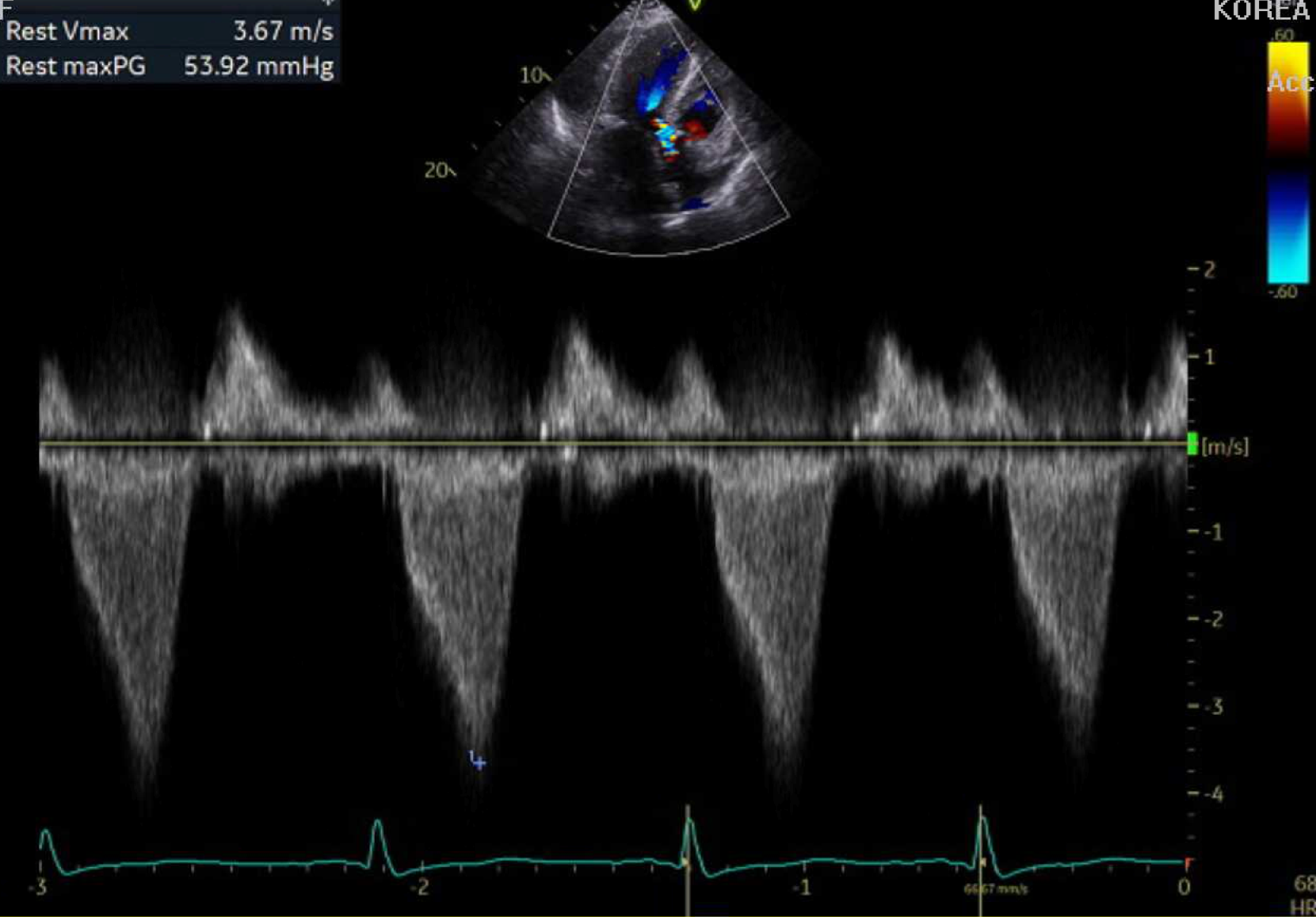
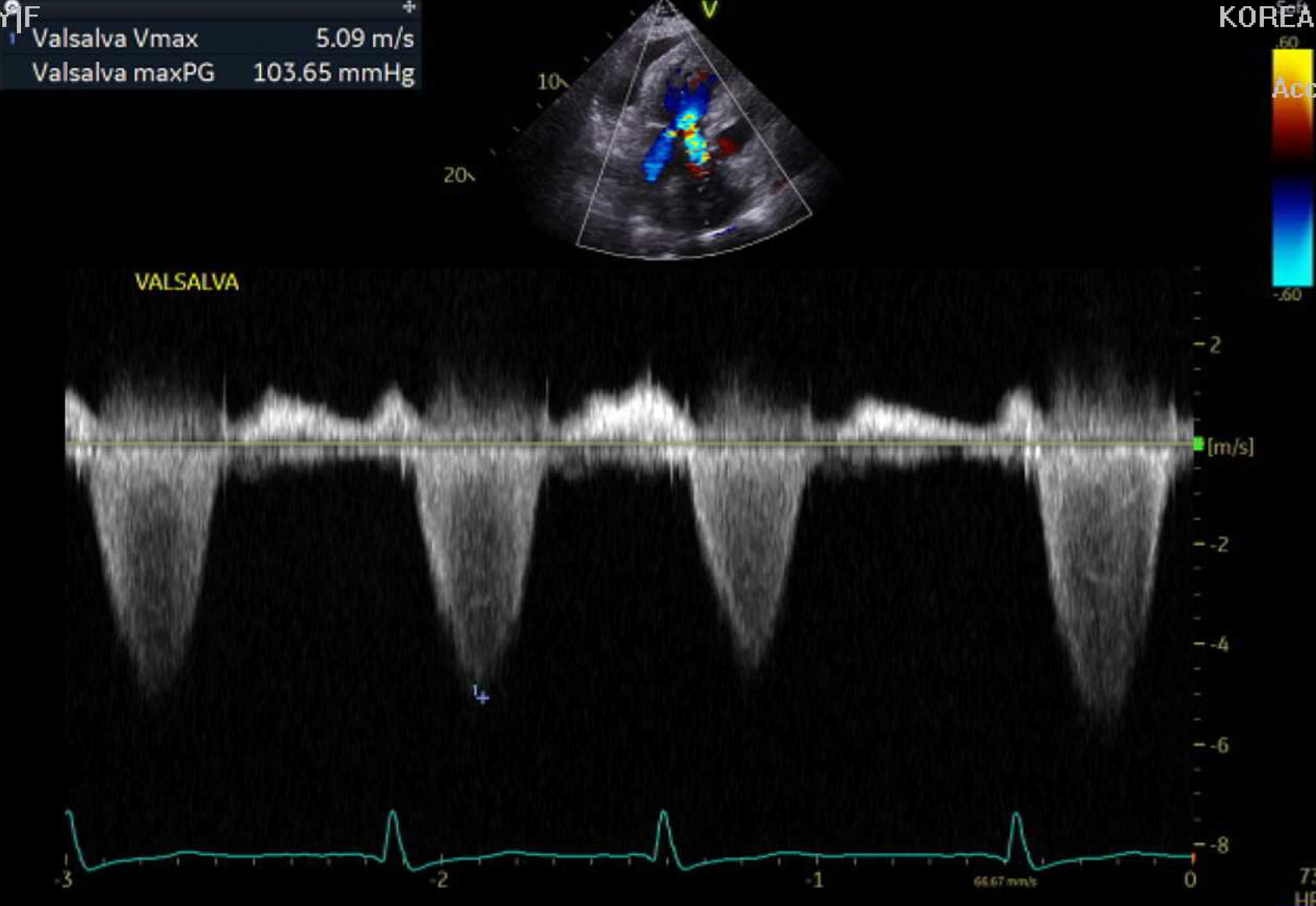
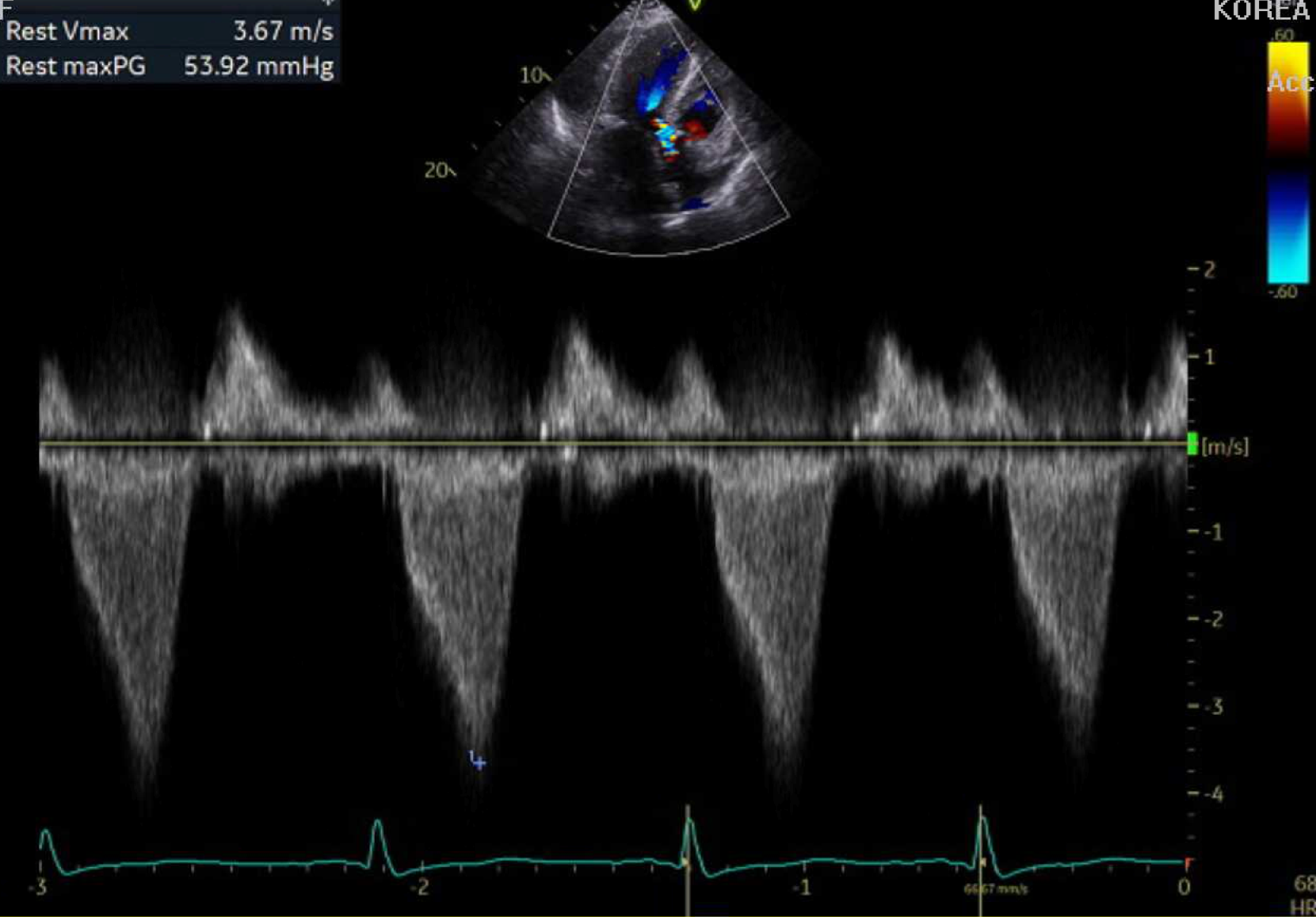
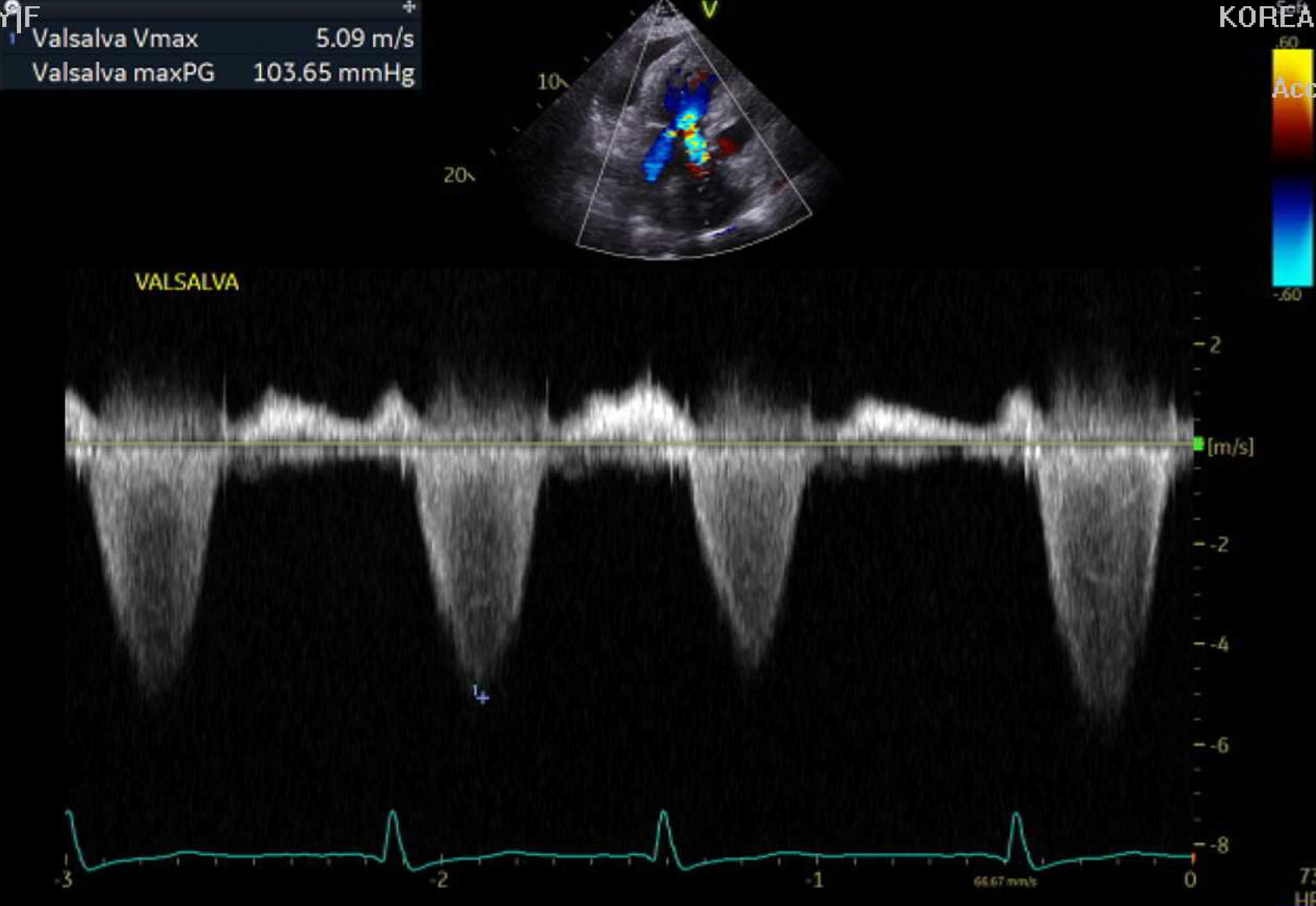
Transthoracic echocardiography demonstrated dynamic left ventricular outflow tract obstruction with baseline peak pressure gradient of 53.9 mmHg, increasing to 103.7 mmHg with Valsalva maneuver. The previously implanted aortic valve prosthesis showed mild paravalvular leak without other significant abnormalities. Additional findings included interventricular septal thickness of 15.9 mm, left ventricular hypertrophy, and preserved left ventricular ejection fraction (55-60%).
Relevant Catheterization Findings
Interventional Management
Procedural Step
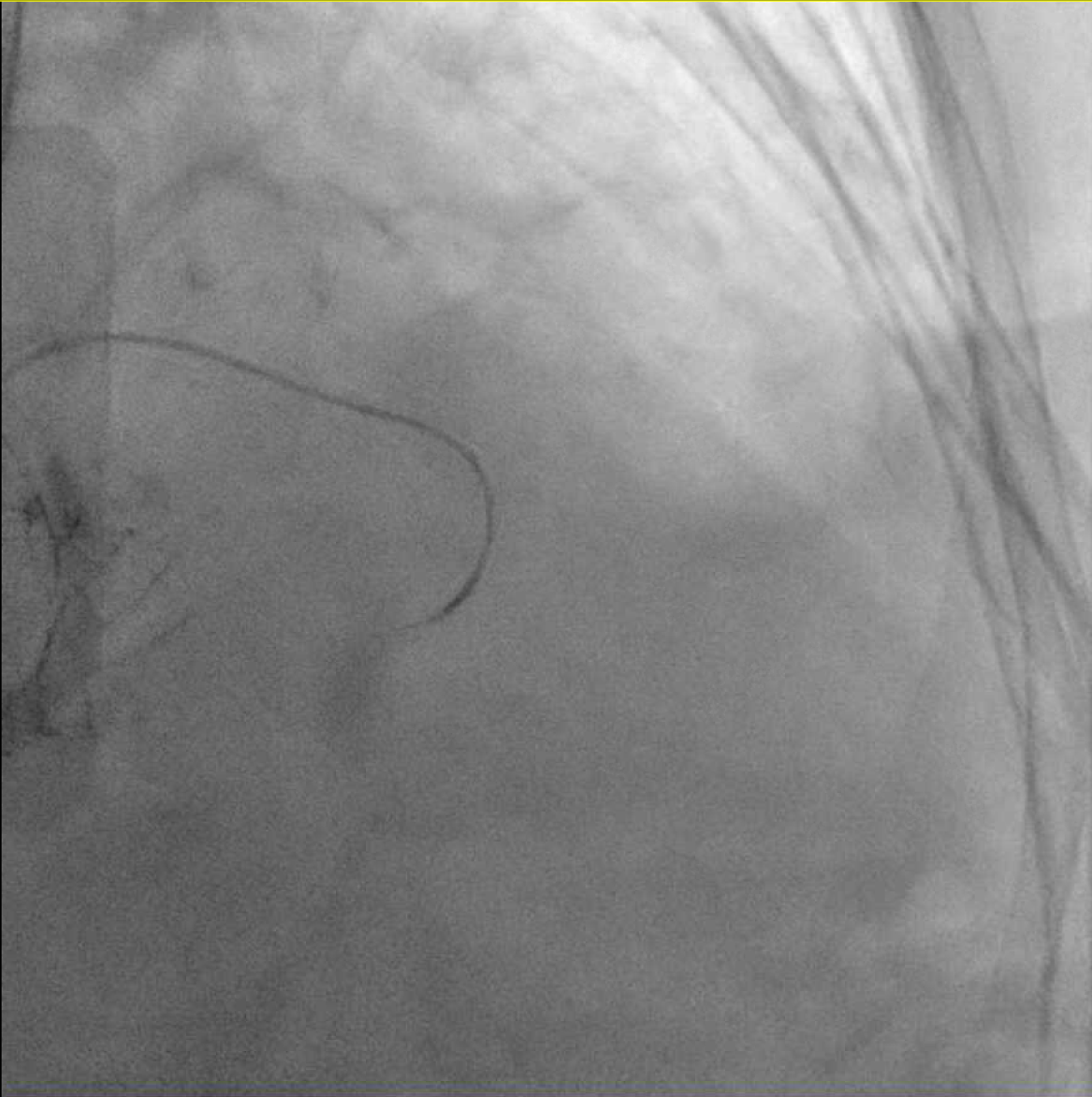
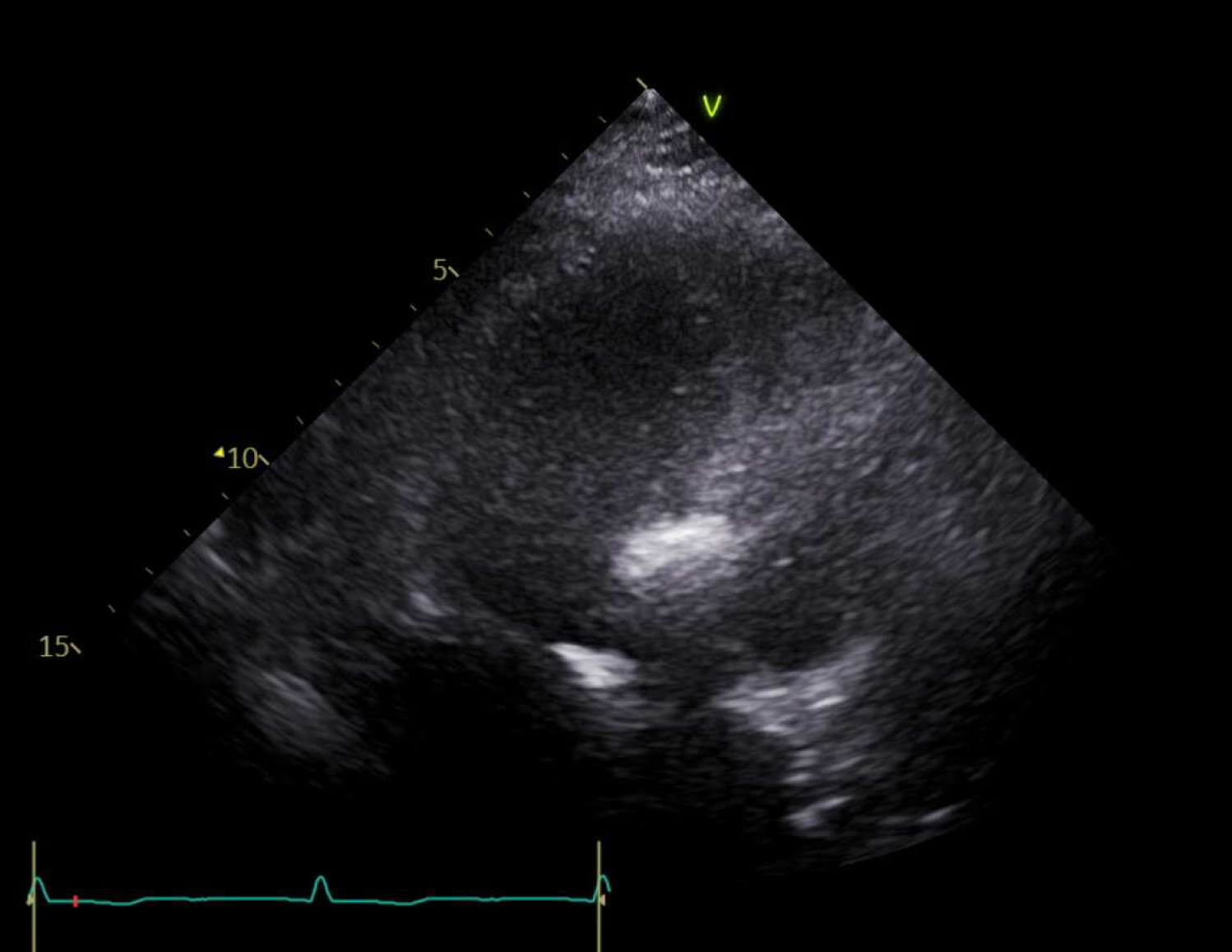
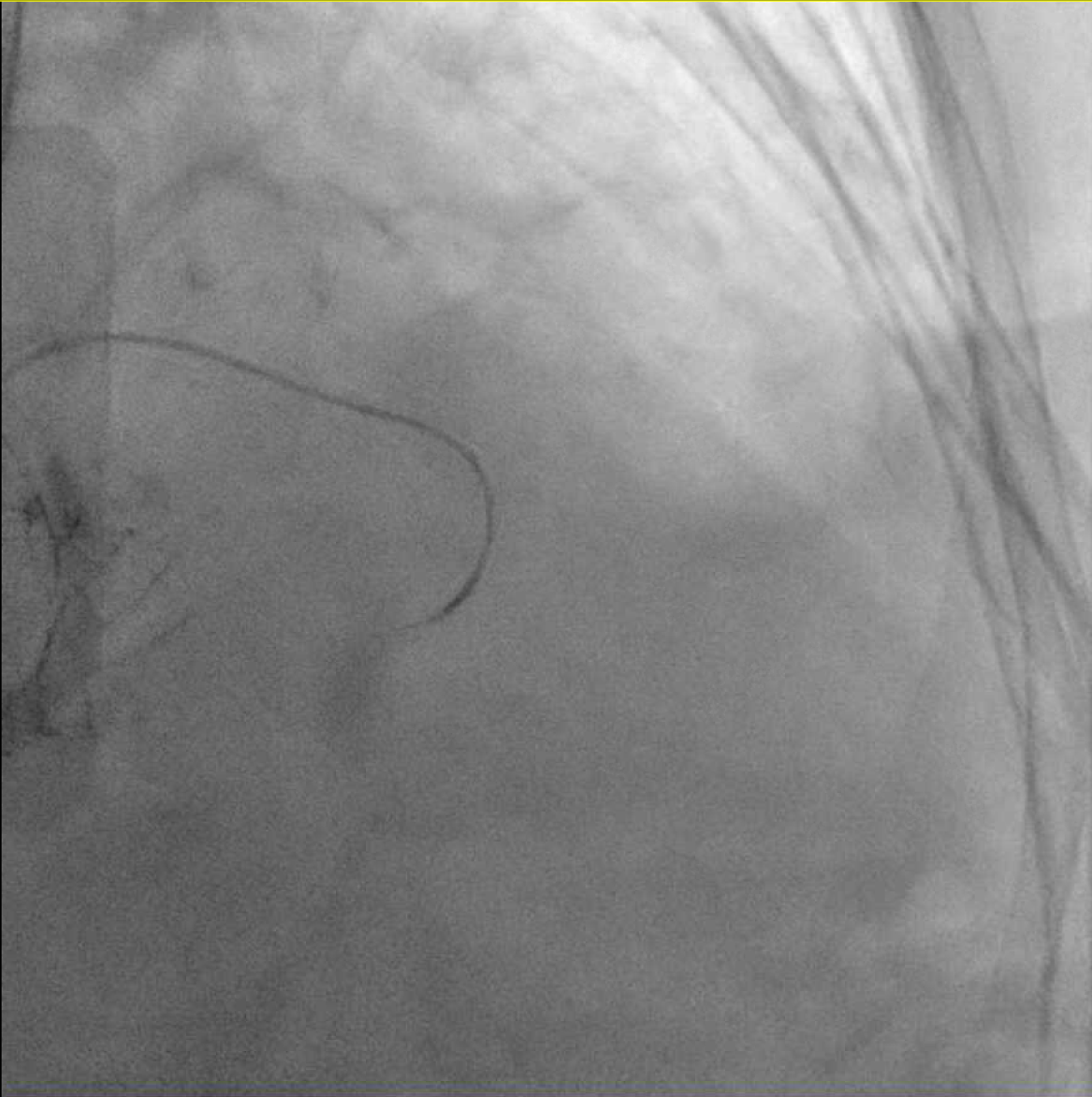
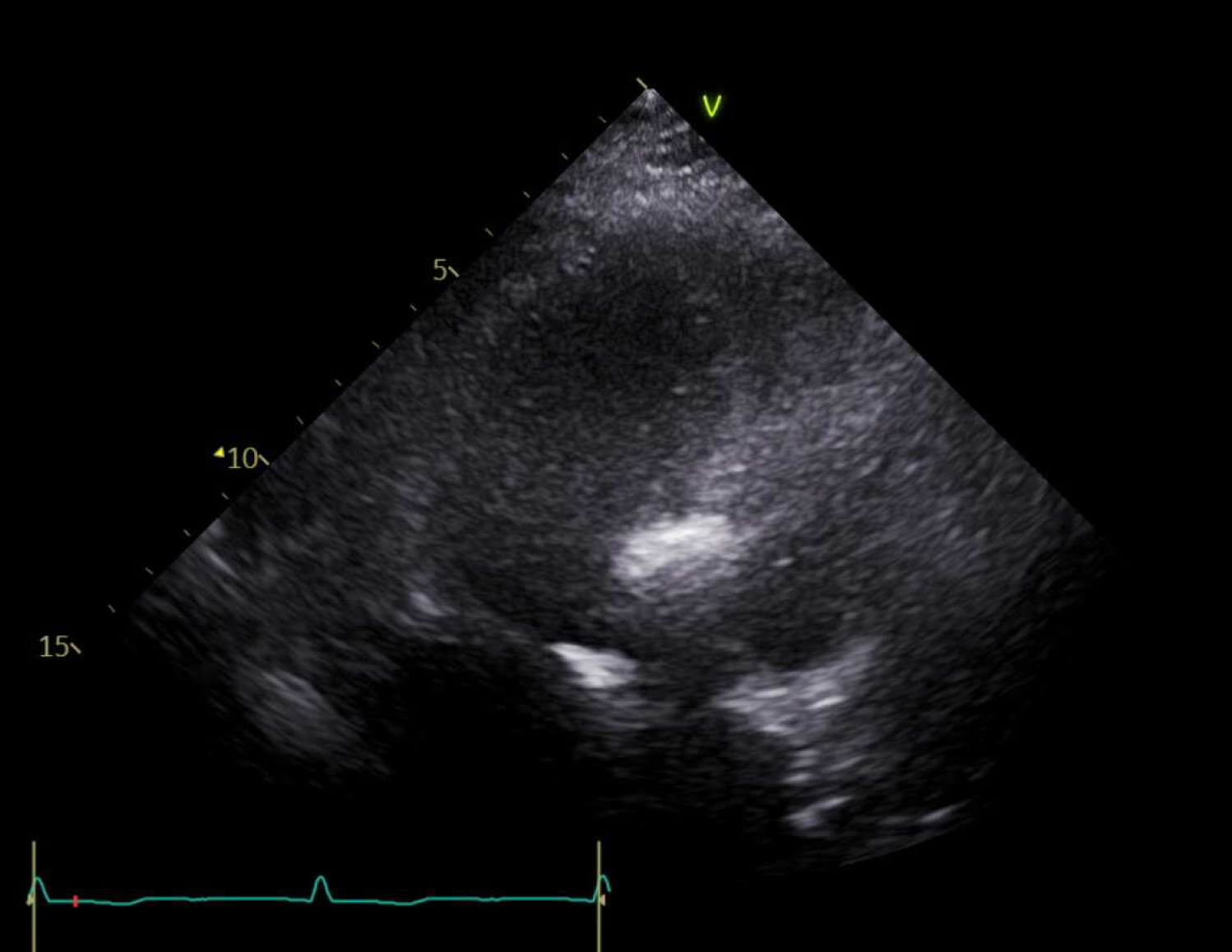
A 6-French (Fr) sheath was inserted into the right radial artery using the modified Seldinger technique. The left main coronary artery was engaged with a 6-Fr JL guiding catheter, and selective injection demonstrated a suitable first septal perforator branch arising from the proximal left anterior descending artery (LAD). A 0.014-inch coronary guidewire was advanced through the guiding catheter and carefully positioned in the target septal branch. Unlike conventional alcohol septal ablation technique, we elected to proceed without using a balloon occlusion approach due to the favorable anatomy of the septal branch. A Corsair microcatheter was advanced over the guidewire and positioned directly in the first septal perforator. Contrast injection through the microcatheter confirmed proper positioning with no retrograde leakage into the LAD and appropriate delineation of the target septal territory. Myocardial contrast echocardiography was performed by injecting 1 mL of diluted echo contrast agent through the Corsair microcatheter to confirm that the target septal branch supplied the area of septal-anterior mitral leaflet contact causing LVOT obstruction. Under continuous hemodynamic andechocardiographic monitoring, 2 mL of absolute alcohol (96%) was slowlyinjected directly through the Corsair microcatheter over a 5-minute period without balloon protection.
Case Summary
This case demonstrates the safety and efficacy of alcohol septal ablation for treating dynamic LVOT obstruction in a post-TAVR patient. Our approach resulted in significant hemodynamic improvement, with reduction of LVOT gradient from 53.9 mmHg to 17.2 mmHg at rest and from 103.7 mmHg to 36.5 mmHg with Valsalva maneuver. Our experience suggests that ASA should be considered in the management algorithm for post-TAVR patients who develop significant dynamic LVOT obstruction, particularly when surgical intervention carries prohibitive risk.
